If you pay attention to your symptoms and don’t continuously aggravate it, you will likely make a full recovery, meaning sciatica is usually temporary.
Sciatica can last anywhere from 2 weeks to 6 months or longer depending on the person. Some people do end up developing sciatica that lasts longer than one year, however, this is a more rare case.
If you get the proper treatment early, the likelihood of having chronic symptoms is very low.
If you’re curious as to all the different causes of lower back pain, you can check out this video and blog post here. (it’s a three part series)
Is Sciatica temporary or permanent?
It’s usually temporary. If you decide to not get early treatment and continue to aggravate it over and over again, it could turn into a more chronic condition.
How long does sciatica last? Is this a permanent disability?
Sciatica can last anywhere between 2 weeks to 6 months or more, depending on severity. Sciatica usually resolves on it’s own over this time period, however you may require more targeted treatment if the pain is becoming unbearable.
Red flags to look out for and when to see your doctor
If you are experiencing progressive numbness, tingling, and weakness of one or both legs, and significant bowel and bladder changes (constipated or unable to hold bladder), please contact your doctor immediately as this could be cauda equina syndrome.
What is the best pain relief strategy for sciatica?
Finding different types of movement that feel best for you is the most important pain relief strategy for your long-term success.
There are many different opinions about what is “best,” but it ultimately comes down to what you enjoy and what doesn’t make the symptoms worse.
Walking, lifting weights, pilates, yoga, swimming, and various other activities are all fine, as long as they do not make symptoms significantly worse.
How do I know how much sciatica pain is okay?
Significantly worse pain would be defined as an hour and 24 hours later the pain has increased by 2 points on a scale of 0-10. If your pain levels are only at 2/10 and it goes to 4/10, I would still consider this to be acceptable. If it goes past a 5, this is when we should start to pay closer attention.
Other strategies to manage acute and chronic sciatic pain
Ice, heat, stretching, TENS, (not too intensely), and massage can all be great tools to help modulate your pain levels. These are modalities that are meant to help you control symptoms and help you get active again.
A combination of modalities (heat, ice, massage), combined with staying active, in addition to giving your body adequate time to heal, is the best-known strategy to improve sciatica.
Unfortunately, there is no secret sauce.
Can the sciatic nerve pinch go away? Is this what’s causing the pain?
Yes, this can go away. Sciatica is often referred to as a pinched nerve. The question though, is whether the nerve is being pinched or not.
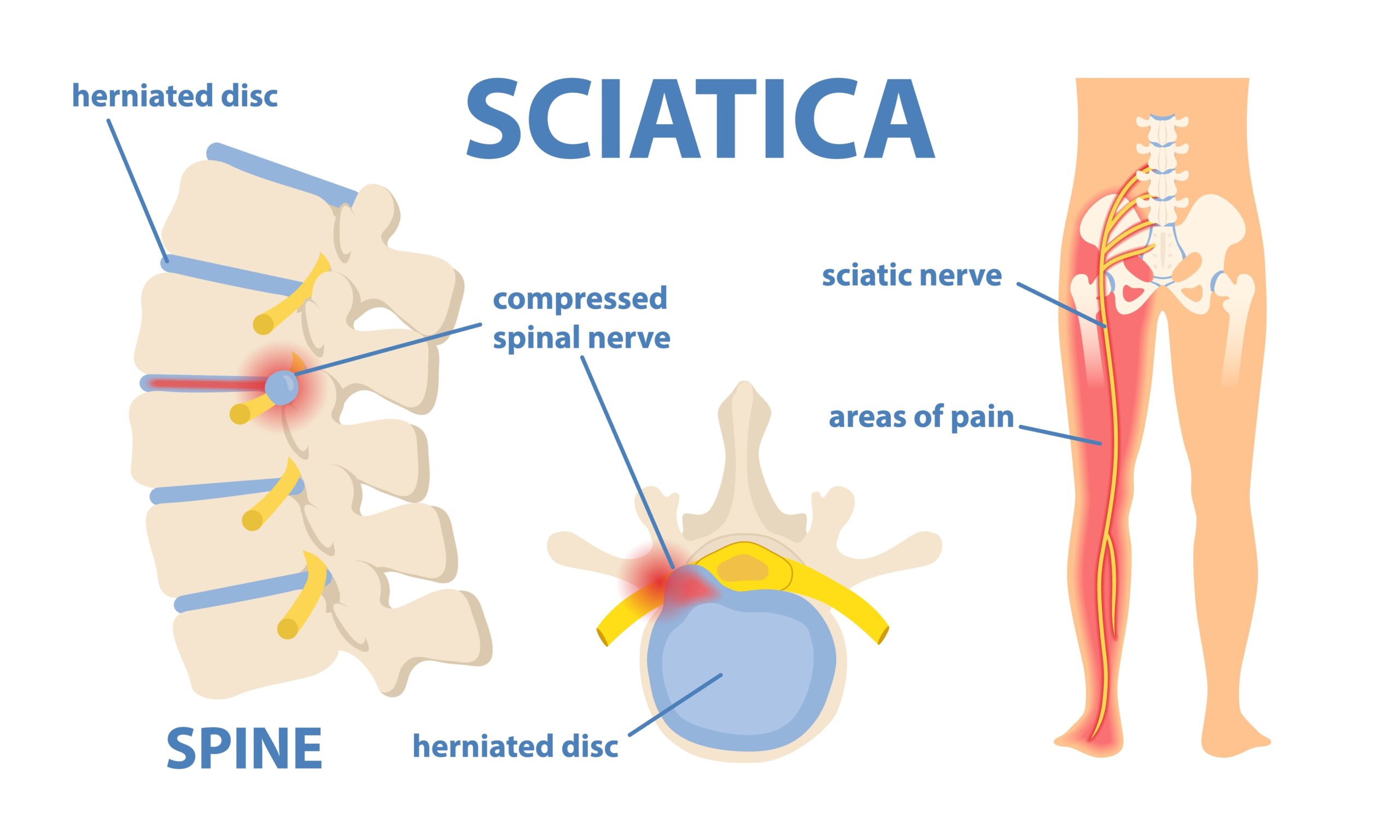
In the instance of a lumbar disc herniation, or stenosis, a pinching or pressing does occur on the nerve root that exits the foramen of the lumbar spine.
What’s interesting about this, is that not everyone who has this pinching or pressing will have pain.
Additionally, some people will experience sciatica pain even without any physical compression of the nerve root.
There is likely some amount of neuroinflammation or inflammation to the nerve root, causing discomfort and pain to travel down the leg.
How physical therapy can decrease pain and how long the sciatic pain lasts
As discussed above, physical therapy can decrease the pain by helping you find movements and types of exercise that do not aggravate symptoms.
Physical therapy can also help you find a management plan of ice, heat, massage, or other modalities that you can do at home to calm your symptoms down when they are acting up.
When Acute Sciatica May Become Chronic
It is possible for sciatica to become chronic and there is a debate among professionals as to when injections or surgery is the best option to address this.
“Chronic pain is pain that lasts more than several months (variously defined as 3 to 6 months, but longer than “normal healing”)
Some professionals suggest that surgery should be considered prior to three months if the symptoms are debilitating as this is when people are likely to have the best results.
If you have gone through three months of non-operative management that was provided by a high-quality therapist and you’ve made no progress or gotten worse, and can’t handle the pain anymore, this may be a good time to consider discussing other options with your physician in an attempt to prevent this from becoming chronic.
In my experience working with clients, I have seen people be successful with therapy, some after 2 weeks, some after 9 months. It really depends on the person.
How to treat sciatica at home
As discussed above, ice, heat, TENS, massage when symptoms are highly irritable, and exercise or movement that does not irritate symptoms more than 2 points on the pain scale.
If you need help developing a game plan for your sciatica you should contact a physical therapist you trust.
You can also join our free facebook group which helps with these issues.
Other medical treatments for sciatica
- Corticosteroid injections – these are 50/50. Some people will benefit, others will not. If the pain is debilitating, they can be worth trying, although some of my clients have reported that it actually made the pain much worse.
- Laminectomy (surgery) – if you are experiencing debilitating pain that is getting worse even after giving it your best effort for several months, then a surgical procedure may be an option for you. There are several types of surgeries, but a laminectomy is the most common. In this surgery they will remove a piece of the bone on your spine that is compressing on the affective nerve root. For the appropriate candidate this procedure can work like magic.
Lifestyle changes
Physical Activity
If this is a recurrent issue for you then lifestyle changes may be in order.
The lowest hanging fruit will be increasing your activity levels. This doesn’t need to be formal exercise, but something as simple as walking 15 to 30 minutes a day can reduce your risk of recurrent sciatica.
Additionally, walking for 15-30 minutes a day will significantly reduce your risk for cardiovascular disease, diabetes, and many other non-communicable illnesses.
It is recommended that everyone gets two times per week of resistance training (lifting weights), however, given so many people ~ 70% of Americans do not get the recommended amount of physical activity, starting with walking is probably a better option.
Sleep
If you are not getting enough, or enough high quality sleep per night, this can also affect your recovery. I recently recorded a podcast with a sleep coach who helps people sleep better without the use of medication. You can find the link here. (link may not be available for a couple weeks as i’m still editing it).
Diet and Nutrition
Add more leafy greens and berries into your diet. This is a quick and easy way to improve how you feel overall.
Additionally, practice mindful eating, checking in with yourself as you are eating and stopping when are satisfied, vs. full. Not only will this help with weight loss if that is your desired goal, but it will also likely help you feel better and not overstuffed.
How is sciatica different from back pain?
Sciatica is a form of lower back pain. Sciatica is also known as lumbar radiculopathy or pain that travels from the back, down one or both legs, front, back or side.
Low back pain or non-specific low back pain (NSLBP) is defined as back pain that does not have a knowable origin. Most back pain is related to NSLBP.
Sciatica can be caused by neuroinflammation of the nerve root itself or compression of the nerve root due to a herniated disc, or stenosis.
Summary
- Sciatica can last anywhere from two weeks to six months or longer depending on the person
- Staying active with activities that do not significantly irritate your symptoms is the best strategy to improve
- Using heat, ice, massage, TENS and other modalities can be helpful to control symptoms when they are at their worst
- Physical therapy can be very helpful in your recovery to help you find the best activities and the correct amount to reduce the chance of a severe flare-up.